What is chemotherapy?
Chemotherapy, also known as a type of systemic anti-cancer therapy or SACT, is the use of drugs to destroy or stop the growth of cancer cells. There are lots of different chemotherapy drugs and they all work in a similar way.
A chemotherapy drug travels through your bloodstream and reaches all parts of your body. This is why it’s called a systemic treatment.
When the chemotherapy drug is in your body, it can either destroy cancer cells or prevent growth by disrupting how they divide and grow. The drug can also affect normal, healthy cells.
Damaged healthy cells may cause you to experience side effects. But most of these are temporary because healthy cells quickly grow back.
How does chemotherapy work?
There are lots of different chemotherapy drugs and they all work in a similar way. The type of chemotherapy drug you have will depend on where in your body your cancer started, how advanced your cancer is and if you’ve previously had chemotherapy. This is because different drugs work on different types of cancer. You may need regular blood tests to assess your overall health and to monitor how your body is responding to chemotherapy during your treatment.
At what stage of cancer is chemotherapy used?
Your consultant may recommend chemotherapy as part of your cancer treatment options for several reasons. These include:
- Using it as the main therapy to treat your cancer
- To shrink a tumour before surgery or radiotherapy (neoadjuvant chemotherapy)
- To reduce the risk of your cancer coming back after surgery or radiotherapy (adjuvant chemotherapy)
- To make cancer cells more sensitive to radiotherapy (often called chemoradiotherapy or chemoradiation)
- To treat or control cancer that has spread to other parts of the body and to ease symptoms (palliative chemotherapy)
How is chemotherapy given?
There are many different ways to deliver chemotherapy, including:
- By mouth as tablets or capsules (oral chemotherapy)
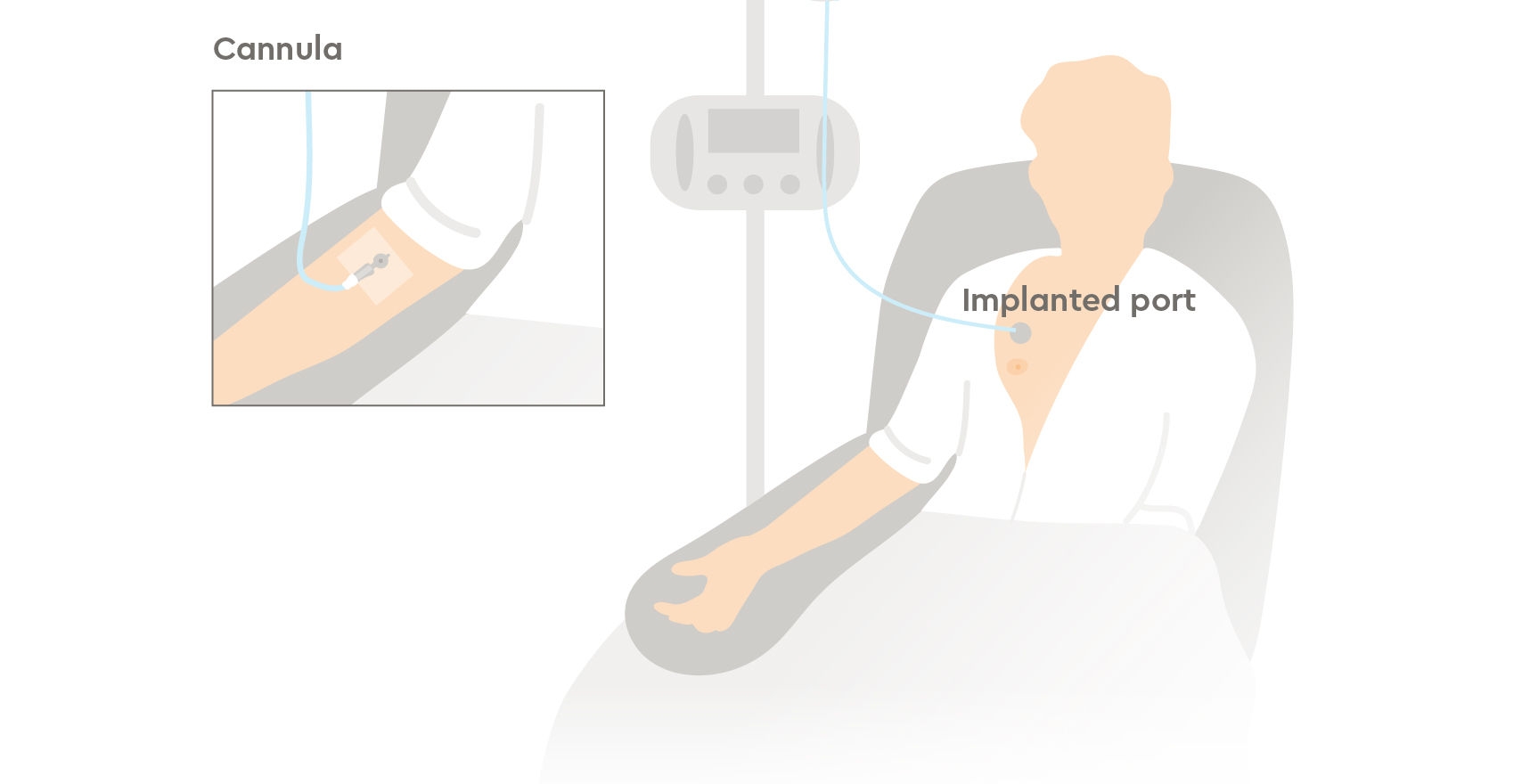
- By injection or a drip directly into a vein via a catheter or cannula (intravenous chemotherapy)
Intravenous chemotherapy can be delivered through a cannula placed into your arm at the start of each session or using a central vascular access device (CVAD) or peripherally inserted central catheters (PICCs), which remains in place until your chemotherapy has finished. Your consultant will explain CVADs in detail, and answer any of your questions, if this is how your chemotherapy will be given.
Other ways you can have chemotherapy are:
- By injection into a muscle (intramuscular) or under the skin (subcutaneous)
- Directly into a body cavity (intracavitary), for example, the treatment of bladder cancer
- Directly to the skin as a cream for some skin cancers
You might have chemotherapy in more than one way. For example, your consultant may recommend you have one type of chemotherapy as a tablet and another as an injection.
How long does chemotherapy take?
Chemotherapy is personalised to you depending on your type and stage of cancer and the drugs you’re receiving. Typically, chemotherapy is given as several treatment sessions through an external infusion pump, with rest periods in between each one.
This is known as a chemotherapy cycle and they’re normally between one to three weeks. A course of treatment can include several cycles and usually takes between three to six months. Each session can range from several minutes up to several hours, depending on the chemotherapy drug you have.
At Genesiscare, our chemotherapy suites are designed to make your treatment sessions calming and stress-free. You’ll be shown to your own restful treatment pod, where you can watch TV, or relax with music. You can bring a friend or family member and refreshments are available.
You’ll receive your treatment as an outpatient, so when you’re ready, you’ll be able to go home after each session.
Chemotherapy side effects
Most common side effects caused by chemotherapy are temporary, but you might be affected by them after your treatment ends. We’ll work closely with you to limit the impact of them as much as possible. Some side effects you may experience include:
- Fatigue (tiredness)
- Reduced immune system and increased risk of infections
- Anaemia due to reduced number of red blood cells
- Bruising or bleeding due to reduced platelets
- Skin and nail changes
- Hair loss
- Digestive problems (Such as nausea, vomiting, diarrhoea or constipation)
- Sex and fertility issues
- Changes to kidneys, liver, heart and lungs
- Changes in hearing
- Nerve damage (peripheral neuropathy)
- Cognitive changes (chemo brain)
Our teams are always on hand to advise you of ways to manage these side effects.
Preparing for Chemotherapy
Preparing for chemotherapy can feel overwhelming, but we're here to guide you every step of the way. We’ll ask you to complete a Macmillan Needs Assessment (MNA) so that our clinicians and nurses can design a personalised care plan and help you meet any challenges and anxieties, confidently and sensitively.
Before starting your treatment, you will also have an assessment appointment which will explain:
- The drugs you will have and how they work, how they’ll be given to you, what side effects you might experience and what to do if they happen.
- The emergency out-of-hours support, including a dedicated 24-hour triage line where our nurses can answer your calls at any time of day or night and quickly assess your symptoms.
We’re dedicated to ensuring that you have all the information and support you need prior to treatment.
Chemotherapy without delay
Chemotherapy, also known as a type of systemic anti-cancer therapy or SACT, is the use of drugs to destroy or stop the growth of cancer cells. SACT is the collective name given to a group of cancer drugs that are used to treat cancer. Other forms of SACT we offer include immunotherapy, hormone therapy and targeted therapies.
Research in oncology and clinical trials have advanced and improved the effectiveness of these treatments, which are delivered by a highly trained multidisciplinary team led by our oncology consultants, to ensure you get the best treatment and care. Oncology consultants are doctors who specialise in the treatment of cancer.
At GenesisCare, we use chemotherapy to treat and manage a wide range of cancers, including breast cancer, bowel cancer, blood cancers and lung cancer.
Leading chemotherapy experts here to support you
If you choose to have your cancer treatment at GenesisCare, your consultant will work with you to develop a personalised care plan based on your specific diagnosis and preferences.
Throughout your chemotherapy, you’ll receive support from a care team of highly trained nurses who are experts in SACTs and managing side effects.
Top-rated cancer treatment
Accredited centres
All our cancer treatment centres have received the prestigious Macmillan Quality Environment Mark for creating friendly and relaxing spaces for people living with cancer.
24/7 oncology nursing
Our compassionate nursing teams are available 24 hours a day on their dedicated emergency service line to answer your concerns, provide advice about side effects and medical care.
Integrative care
We give every patient access to therapies that are proven to improve outcomes for people diagnosed with cancer, including psychological support and exercise medicine.


Our patient stories
Read firsthand experiences of patient care through chemotherapy treatment at GenesisCare.
Chemotherapy FAQs
We have put together a list of commonly asked questions about chemotherapy. If you have a question that isn’t answered below, please contact us, we’re always happy to help.
The best form of treatment for you will depend on many factors like your type of cancer or the stage of your cancer.
Chemotherapy is a medicine designed to destroy cancer cells and can be given in a number of ways, such as in tablet form or through a vein (intravenously).
Radiotherapy uses radiation beams directed at the tumour and is focused on one area of your body.
Your consultant will always discuss your options with you and help guide you to the best treatment options for you. Often, chemotherapy and radiotherapy can complement each other and be used together. This is known as concurrent therapy and may be suggested if your cancer is:
- Difficult or unable to be removed through surgery
- There is a risk of the cancer spreading
- The cancer is not responding well to other forms of treatment
Chemotherapy and immunotherapy are both treatment options for cancer, but they work in different ways. Both are effective in treating cancer, and your consultant will discuss with you the best option for you and your particular case. Sometimes you may be given a combination of immunotherapy and chemotherapy, this is called chemoimmunotherapy.
While chemotherapy kills cancer cells, immunotherapy encourages your immune system to recognise and fight cancer cells.
Your immune system is already designed to protect your body from infections and cancer. However, cancer cells can sometimes hide or trick your immune system from attacking them, making it more difficult to naturally fight them. Immunotherapy helps your immune system to recognise cancer cells and become more effective at destroying them.
Learn more about how immunotherapy works and how it’s given.
Traditional chemotherapy drugs are not usually thought of as targeted because they don’t specifically attack cancer cells.
However, the chemotherapy drugs damage any rapidly dividing cells within your body, as cancer cells divide quickly, the chemotherapy attacks them first. Occasionally, some healthy cells that also divide quickly, can also get caught by the chemotherapy drug. This is what causes side effects.
Targeted therapy drugs focus on cancer cells, and they often work by stopping cancer cells from copying and making new cancer cells.
Learn more about how targeted therapy works and how it’s given.
When we say a chemotherapy dose, we’re talking about the amount of each individual drug that you’ll receive. A chemotherapy cycle refers to the set period of days you’ll be given your chemotherapy.
The length of a cycle will vary between one to three weeks, including rest breaks during a cycle. A course of treatment refers to your whole chemotherapy treatment and is made up of a planned number of cycles.
Chemotherapy treatment typically ranges from a few minutes to several hours. Some treatments can also be given continuously over a couple of days. It’ll depend on a variety of factors, such as the amount of chemotherapy you’ve been prescribed, how you’re having your chemotherapy and the type of cancer you have. Your consultant or care team will be able to give you a clearer idea of how long a chemotherapy session might take.
Having chemotherapy shouldn’t be painful. It might be uncomfortable, for example, while your nurse is inserting the needle (if you’re having treatment intravenously). If you find this painful, let your nurse know.
Most of the discomfort that can be felt from chemotherapy is from the side effects you may experience afterwards. Pain can be a side effect of chemotherapy, and some patients report the feeling of tingling, shooting or numb sensations in their hands and feet. This is called neuropathic pain, and it happens because of nerve damage caused by the chemotherapy drugs.
You may get headaches, muscle or stomach aches, but these should be manageable. However, if you’re finding it difficult to manage the pain, please speak to your consultant. They should be able to help you either by adjusting your dose or prescribing you medicine to help ease the pain.
Absolutely! You may not always feel up to exercising during your treatment, but studies have shown that even mild exercise during treatment can help in a variety of ways. It can help your body heal itself, improve the effectiveness of some treatments and speed up your recovery.
It can also help improve your quality of life after treatment and reduce the chance of cancer returning. Before taking up any new exercise plan, you should first speak to your consultant to find out the best level of exercise you should be aiming for.
At GenesisCare, we offer integrative cancer care, which includes our exercise medicine programme, where one of our dedicated physiotherapists will develop a 12-week exercise plan personalised to you and your needs, side effects, and the goals you want to achieve.
The cost of chemotherapy treatment is dependent on several factors, as it is tailored to each unique medical situation. Variables such as diagnosis, the type of drugs prescribed, the length of treatment needed, as well as additional medical considerations all play a role in determining the cost. Our team is committed to providing transparent information about these factors.
We’re recognised by all major insurers, including Bupa, AXA PPP, Aviva and Vitality who usually cover all associated costs of treatment. Self-pay options are also available, where we ensure you have a clear understanding of the financial aspects of your treatment journey. We're here to support you every step of the way.
Chemotherapy drugs work by damaging any rapidly dividing cells within your body and as cancer cells divide quickly, the chemotherapy attacks them first. Some healthy cells that also divide quickly, such as those in hair follicles, can also get caught by the chemotherapy drug, disrupting the hair growth cycle.
This can lead to hair thinning or hair loss, with hair typically growing back after treatment ends. Our team is here to provide support and guidance throughout this process, helping you navigate any changes with confidence and dignity.
Reviewed by: Dr Karthik Ramasamy
Haematologist
October 2024

