What is stereotactic radiosurgery?
Stereotactic radiosurgery, or SRS, is an advanced radiotherapy technique that precisely delivers multiple beams of radiation to a tumour, sometimes in one single treatment session. Despite its name, SRS is not surgery – it doesn’t involve any incisions and the procedure is painless.
SRS is often referred to as a ‘brain-sparing’ radiotherapy approach as it’s widely recognised for its ability to preserve the quality of life in people with cancers that have spread to the brain (brain metastases).
We offer SRS as part of our comprehensive state-of-the-art neuro-oncology service in Oxford and London. This also includes an array of advanced diagnostics and planning techniques that enable us to create your own tailored treatment plan. Our neuro-oncology service is underpinned by leading professionals and world-class technology so that we can offer exceptional care and maximise your chance of the best possible outcomes.
Make an enquiry
If you’d like more information about our specialist stereotactic radiosurgery service, just get in touch.
SRS versus conventional brain radiotherapy
Conventional radiotherapy for the treatment of brain tumours involves high-energy X-ray beams that deliver a prescribed dose of radiation directly to your tumour cells. The aim is to shrink your tumour and stop it from growing. If you have several small tumours (metastases) the radiation is often directed across the whole brain area.
SRS uses narrower X-ray beams which are from different angles. As a result, SRS can target small tumours with exceptional accuracy while avoiding the surrounding healthy brain tissue. Because of this greater accuracy, we are able to deliver higher doses of radiation to the tumour site and minimise the side effects you’ll experience.
The three main advantages of stereotactic radiosurgery (SRS) over conventional radiotherapy are:
- Single treatment
You may need as many as 10 treatments with conventional radiotherapy. But with SRS, the radiation is far more powerful and can be delivered in as little as a single dose, allowing you to get on with your day-to-day life. - Reduced side effects
Increased accuracy means the radiation beam is less likely to hit your healthy tissue – and so less likely to cause long-term side effects. Several studies have shown that this can help to preserve everyday cognitive function and an improved quality of life after treatment. - Less likely to need conventional surgery
In many cases, SRS can be used in place of conventional surgery. This means no invasive treatment, no scarring, a quicker recovery period and little risk of infection.
What happens during SRS?
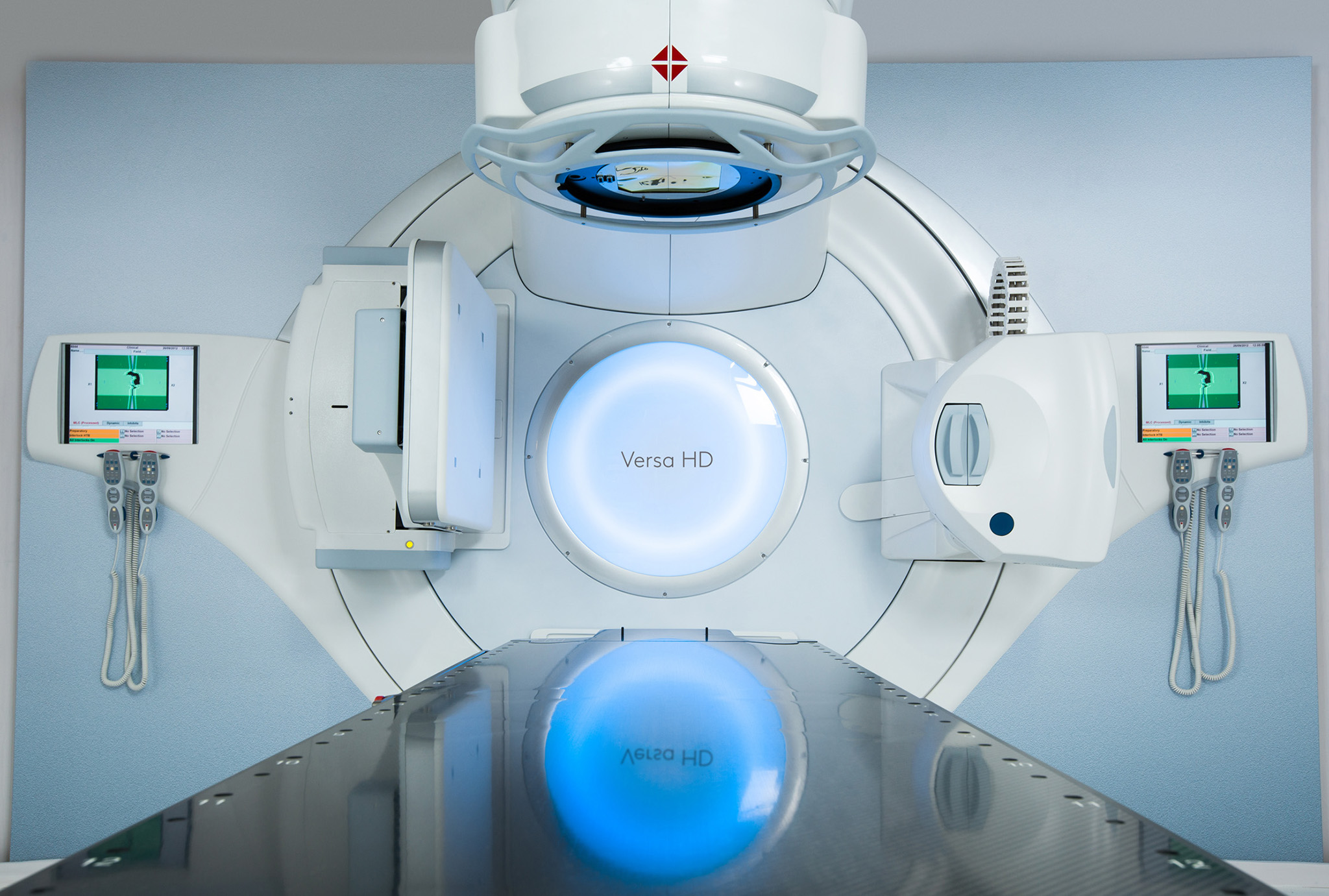
SRS can be delivered using many different advanced technologies. We use a linear accelerator (linac) and X-ray radiation at our centres in Oxford and London. Our centre in London also has a Gamma Knife which uses gamma rays. Both these techniques are equally effective in treating brain metastases, but there are some differences in the planning and treatment for each.
Follow this link if you want more information about Gamma Knife radiosurgery at our GenesisCare Centre for Radiotherapy at Cromwell Hospital
Here’s what to expect during your SRS treatment plan in Oxford and London using a linear accelerator – including before, during and after the procedure.
Face mask fitting
For your treatment you’ll need to be fitted with a custom-made mask that keeps your head still during the treatment. This helps limit damage to your healthy brain tissue. Sheets of plastic mesh that has been softened in warm water will be placed over your face and head and moulded to fit you. They will harden as they dry over 45 minutes. Don't worry, you'll be able to breathe normally.
CT and MRI scan
To help your care team plan your treatment, you will need a CT (computerised tomography) and MRI scan so they can locate the exact size, shape and position of your tumour. This information is fed directly into the radiotherapy planning computer.
Functional MRI scan
You may also have an fMRI scan to enable your team to locate the areas of your brain that are involved in movement or speech.
Before your treatment begins, you may be given steroids to help minimise the risk of swelling in the area of your brain that is being treated. You will usually remain on steroids for the duration of your treatment and be taken off these gradually once your treatment is complete. Once you’re ready, you’ll be helped into position on the treatment couch and your radiographers will fit your custom face mask from your planning appointment.
Your radiographers will leave the room for the duration of the procedure, but they’ll be monitoring you at all times and you’ll be able to talk to them via an intercom.
You won’t be able to feel anything during treatment as SRS is completely painless. Your session may take between 20 to 60 minutes, though this can be a little longer for more complex cases.
When the treatment has finished, your radiographer will come back into the room and help you off the couch. You’ll be able to go straight home, however, you wont be able to drive due to DVLA regulations – your consultant will discuss this in more detail with you.
Your doctor will let you know what your follow-up schedule will be, depending on the number, size, location and prognosis of your tumours.
After your treatment course has finished, a member of your care team will call you to check on your recovery at weeks one, two, four and six. You’ll then have a review after four to six weeks with your consultant, and a follow-up MRI of your brain to see how the treatment has worked two to three months later.
Who is suitable for SRS?
SRS may be suitable for you if you have either a tumour that starts in your brain (primary tumour) or a tumour that has spread from elsewhere in your body (metastatic or secondary tumour). This includes:
- If you’ve had surgery to remove brain metastases to reduce the risk of recurrence
- Small tumours such as pituitary adenomas and chordomas or meningiomas at the base of the skull
- Benign (non-cancerous) tumours such as acoustic neuromas (vestibular schwannomas)
SRS may not be suitable if:
- The treatment area includes certain important nerves that could be damaged by radiation
- Your tumour is larger than 3cm across
Our clinicians are experts in the use of SRS as well as other techniques and will decide if this is the best option for you after careful evaluation of your condition.
Possible side effects
Stereotactic radiotherapy is a well tolerated treatment with greater accuracy than conventional radiotherapy.
Not everyone experiences side effects but your risk may be affected by your general health, other treatments you’ve had and the location of your lesion or tumour.
If you do experience some changes after treatment, your care team will advise you on the best way to deal with them.
You may experience the following side effects during your treatment course. Short-term side effects last for a few weeks (four to six) after treatment.
Common side effects:
- Fatigue
- Headaches
- Dizziness
Less common side effects:
- Nausea/vomiting
- Skin changes and hair loss in the area of treatment
- Temporary worsening of your symptoms
- Seizures*
* Risk of seizures is slightly increased after treatment but usually only affects people who have a history of seizures. Ask your medical team for advice. If you have a seizure for the first time, go straight to your nearest hospital’s accident and emergency department.
Around 10% of people notice side effects months, or even years, after SRS. These are likely to be related to the areas of the brain that are being treated and your doctor will guide you through these. They may include:
- Short-term memory loss
- Cognitive function
- Radiation damage to the normal brain
- Risk of secondary cancer years later, though this is rare
- Damage to pituitary gland
- Visual impairment
- Hearing loss
Some of these side effects can be successfully treated. It’s important that you inform your clinical team and to attend your follow-up visits and scans so side effects can be identified and treated early.
If you have a primary or secondary brain tumour, you may have to notify the DVLA. You may not be allowed to drive for a certain period of time depending on the type of tumour and treatment received. Your doctor can advise you further.
Our multidisciplinary team
We have specially selected a neuro-oncology multidisciplinary (MDT) team that brings together the expertise of neuro-radiologists and neuroimaging scientists, alongside neuro-oncologists and neurosurgeons. This dedicated team will review all referrals to our neuro-oncology service, meaning your care will be planned by a team of experts to ensure you get the best treatment tailored to your needs. The members of our neuro-oncology MDT are listed below.



Dr Fintan Brian John Sheerin
MA hons Cantab Physiology MB, Bchir hons Cantab MRCP UK FRCR
Neuroradiologist
Oxford

Dr Pieter Michiel Pretorius
MBChB (University of the Free State) MSc (OXON) FRCR
Neuroradiologist
Oxford