What is pancreatic cancer?
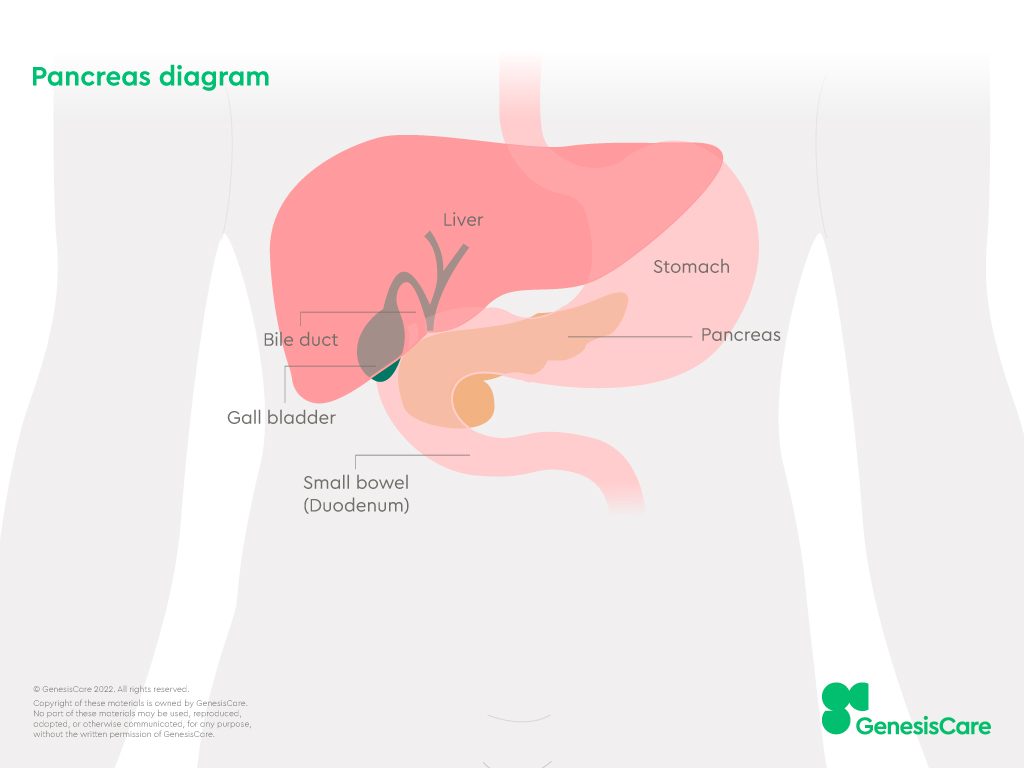
The pancreas is located next to the liver, duodenum and stomach where it produces enzymes to help digest food (pancreatic juice) and hormones (including insulin).
Most pancreatic cancers are ductal adenocarcinomas, meaning cancer cells that start in cells lining the ducts. Pancreatic cancer cells can spread elsewhere in the body through the blood and lymphatic vessels, becoming metastatic or advanced pancreatic cancer.
Pancreatic cancer is the 10th most common cancer in the UK. According to Cancer Research UK, there are around 10,300 new cases of pancreatic cancer each year. It mainly affects people over the age of 60, and almost half of people who have pancreatic cancer are at least 75.
Where is your pancreas?
The pancreas is deep in the centre of your abdomen. It’s around 6cm long and shaped like a leaf.
It’s tucked into a curve in the small intestine and makes enzymes/fluids to help break down food as it passes through your intestines.
The pancreas is also connected to blood vessels. It secretes hormones like insulin and glucagon into the blood, which help control your blood sugar.
Early signs and symptoms
Symptoms of pancreatic cancer often appear late. They can also be vague, which makes it a complex condition to diagnose. It helps to know the signs and symptoms so that you can act quickly if you notice them.
The most common symptoms of pancreatic cancer are:
- Back pain
- Stomach pain
- Unexpected weight loss
- Losing your appetite
- Jaundice – yellowing of the skin and whites of the eyes
- Extreme tiredness
Other signs of pancreatic cancer may include:
- Itchy skin
- Nausea and vomiting
- Changes in bowel habits
- Diabetes
- High temperature
- Indigestion
- Blood clots
When to see a doctor
If you notice any symptoms that could be related to pancreatic cancer, it’s important to see a doctor straight away. It might not be cancer, but it’s always better to get checked so any treatment can start without delay.
You can see your GP, who can refer you to a specialist if appropriate.
Types of pancreatic cancer
Several types of pancreatic cancer exist. The type depends on the cells where the cancer started and affects your symptoms, treatment, and overall outlook.
Pancreatic tumours can be:
- Exocrine cancer starts in cells that make enzymes
- Neuroendocrine cancer starts in cells that make hormones that help control how our bodies work
95% of people with pancreatic cancer have an exocrine type called pancreatic ductal adenocarcinoma (PDAC). General information about pancreatic cancer is usually referring to this type unless it says otherwise.
PDAC starts in the cells lining the pancreatic ducts. These are the small tubes connecting the pancreas to the small intestine. Vague symptoms of PDAC often lead to a late diagnosis, but if caught early, a cure is sometimes possible with surgery.
Acinar cells are attached to the pancreatic ducts and are responsible for making enzymes. This type of exocrine pancreatic cancer is more common in younger people. It tends to grow more slowly than PDAC, which can mean an improved outlook.
Cystic tumours start as benign fluid sacs (cysts) in the pancreas that can become cancerous. The main treatment is surgery, which may have a good outlook compared to other exocrine cancers.
Also known as neuroendocrine tumours or islet tumours. Endocrine pancreatic cancer is rare. The symptoms depend on the hormones affected and can include blood sugar related symptoms, diarrhoea, and severe stomach pain.
Pancreatoblastoma and pancreatic sarcoma are very rare types of cancer. At GenesisCare, we treat all types of adult pancreatic cancer.
What causes pancreatic cancer?
Usually, it’s not possible to pinpoint why someone develops pancreatic cancer. But risk factors increase your chances of being affected.
Your risk of pancreatic cancer increases if:
- You’re aged 60+
- You smoke tobacco
- You have a high BMI (over 30)
- You have a family history of pancreatic cancer
- You have type 2 diabetes
- You have chronic pancreatitis
- You’re exposed to certain chemicals in your job
Certain gene mutations and conditions can increase your risk of pancreatic cancer. These include BRCA1, BRCA2, ATM, and PALB2. Other risk factors are hereditary pancreatitis, Lynch syndrome, and Peutz-Jeghers syndrome.
Enquire now
If you’d like to find out more, please contact us today. We’re always happy to answer any questions and concerns you may have.
Diagnosis and tests
How is pancreatic cancer diagnosed?
Your doctor explores what’s causing your symptoms with several tests and scans, including ruling out other benign conditions. The first step is usually to have urine and blood tests, a physical exam, and a CT or ultrasound scan. If your results show possible signs of cancer, they’ll refer you for more specialist tests. These tests and scans include:
- Biopsy – taking a sample of pancreatic tissue to test for cancer cells
- Endoscopic ultrasound – looking inside the body to create detailed images of the pancreas, stomach, and gallbladder so that a biopsy can be taken from the correct area
- Endoscopic retrograde cholangio-pancreatography (ERCP) - uses medical dye and X-rays to create detailed images of the pancreas, liver, bile ducts and gall bladder and can be used to unblock the bile duct if obstructed by tumour
- MRCP – A specialised MRI scan that creates detailed pictures of your pancreas, gallbladder and bile ducts using magnetic fields
- PET-CT – an imaging scan that uses a radioactive dye that binds to highly active cells, to show areas of cancer throughout the body
- Tumour marker tests – a blood test to measure proteins released by pancreatic cancer cells such as CEA and CA19-9
Prevention of pancreatic cancer
It’s not always possible to prevent pancreatic cancer, but there are positive things you can do to lower your risk.
- Stop smoking – 1 in 5 cases of pancreatic cancer are caused by smoking, according to Cancer Research UK
- Aim for your healthy weight range – keeping your BMI under 25 can lower your risk of pancreatic cancer, among others
- Lower your risk of type 2 diabetes – this common condition can be prevented by being active regularly and eating well
- Stick to the recommended alcohol limit – this helps lower your risk of chronic pancreatitis, which is linked to pancreatic cancer
Pancreatic cancer treatment overview
There are treatments for all stages of pancreatic cancer. Some early-stage pancreatic cancers can be cured with surgery. When surgery isn’t an option, treatment aims to control your cancer – helping you live as well as possible, for as long as possible.
At GenesisCare, it’s our commitment to offer world-class care to every patient with cancer. Skip ahead to discover our treatment approach.
How is pancreatic cancer treated?
The primary treatments for pancreatic cancer include surgery, which involves removing part or all of the pancreas; chemotherapy, where anti-cancer (cytotoxic) drugs are used to destroy cancer cells; and radiotherapy, which targets cancer cells with high-energy radiation beams.
Surgery is the main treatment for early-stage pancreatic cancers. It can be part of an overall care plan alongside other treatments.
Pancreatic cancer surgery can use various procedures. Your surgeon will recommend the most appropriate technique depending on the size, location and spread of your cancer.
Other procedures can help relieve symptoms if your cancer is blocking the bile duct or part of your small bowel.
Systemic anti-cancer therapies are treatments, such as chemotherapy, that target cancer cells throughout the entire body.
Chemotherapy uses cytotoxic (anti-cancer) drugs to slow the growth of cancer cells. It can be given on its own or in combination with radiotherapy (chemoradiation).
Chemotherapy or chemoradiation can be given before surgery to reduce the size of your pancreatic tumour before the operation, called neoadjuvant treatment.
It may also be given after surgery to prevent cancer from coming back. Chemotherapy is also used when pancreatic cancer has spread to other organs.
Radiotherapy can be given to treat pancreatic cancer or help relieve symptoms of advanced disease. You might also have radiotherapy in combination with chemotherapy (chemoradiation), before or after surgery.
Specialised techniques help limit side effects by targeting radiation to cancer cells while avoiding healthy cells. Advanced technologies, including stereotactic ablative radiotherapy (SABR) delivered on the MRIdian MR linac which can target tumours with millimetre precision, improving treatment accuracy and reducing side effects.
Learn more about advanced radiotherapy available from GenesisCare.
Palliative cancer care aims to control cancer and ease symptoms. The treatment helps shrink and slow down advanced cancer that has spread, known as metastatic cancer.
For pancreatic cancer, this can include palliative radiotherapy or chemotherapy.
For some advanced cancers, specialist tests such as liquid biopsy or genomic testing are used to understand the genetic makeup of cancer cells. This helps identify which drugs could work against the particular genetic mutations in a cancer.
There may also be opportunities to access clinical trials for the newest treatments for pancreatic cancer.
Pancreatic cancer treatment at GenesisCare
We are the UK’s leading independent provider of private cancer care. By choosing us, you can be reassured that your treatment is managed by a team of specialists working together with you to design the best plan for your pancreatic cancer.
Our approach to world-class care for pancreatic cancer includes:
- A personalised plan built around you
- Treatment starting within days if needed
- 14 outpatient cancer centres across the UK
- State-of-the-art facilities specialising in advanced radiotherapy
- Compassionate chemotherapy nurses available 24/7 by telephone
- Integrative cancer care including wellbeing therapies and exercise medicine
- We're recognised by all leading private medical insurers with self-pay options available
- Transport provided, depending on location and treatment
We are proud that so many patients rate our care as excellent as we help them through their cancer journey. Hear the unique experiences of people who have had their cancer diagnosis or treatment at GenesisCare in our patient stories section.
Surgery
Our consultants include expert surgeons who work in local and nationally renowned hospitals. They collaborate with other cancer specialists to tailor a treatment plan for you.
If your consultant recommends pancreatic cancer surgery, this can be arranged conveniently at one of our comfortable partner hospitals. You can then continue any other treatments at GenesisCare.
Systemic therapy
We offer all types of drug therapies used to treat and manage pancreatic cancer, including many of the newest treatments. Depending on the treatment, you may attend one of our private suites staffed by our specialist nurses.
Our compassionate nursing teams are available 24/7 on a dedicated on-call telephone service and can answer any queries during your treatment. They’ll be able to provide advice about side effects or symptoms and arrange any care you need throughout.
Our centres have all received the Macmillan Quality Environment Mark to reflect the quality of care we provide for people living with cancer.
Radiotherapy
At GenesisCare, we’re equipped with the UK’s first MRIdian MR Linac machines at our centres in Oxford and Cromwell Hospital London. The MRIdian delivers MRI-guided stereotactic ablative radiotherapy (SABR) combining magnetic resonance imaging (MRI) with live images to see exactly where a tumour is at the same time as treating it. This next-generation technology automatically shuts off the radiation beam when the tumour moves.
This highly accurate form of radiotherapy can be used be used to treat pancreatic cancer that has spread to a small number of other areas of the body, such as the liver, lung or lymph nodes. It can also be used to treat inoperable pancreatic cancer by controlling tumour growth or reducing tumour size to enable surgery.
MR-guided SABR can also be used in patients who have previously undergone radiotherapy. This is known as SABR reirradiation (also referred to as repeat SABR). For people with pancreatic cancer, fast treatment is essential as they can become ill very quickly. That’s why we offer a rapid access pathway for those with pancreatic cancer that hasn’t spread outside the pancreas.
Eligible patients can start treatment within seven to ten working days of their oncologist agreeing treatment with them, and the referral being received. This approach maximises the chance of getting the best outcome from treatment and is available to patients with private medical insurance and those wishing to self-fund their care.
We also offer:

Find out more about MR-guided radiotherapy for pancreatic cancer.
FAQs about pancreatic cancer
Sometimes pancreatic cancer can be cured by removing the whole pancreas, which is a surgery called total pancreatectomy.
It’s possible to live without a pancreas, but you’ll need lifelong treatment, including taking insulin to control your blood sugar and enzyme capsules to digest your food. It’s a life-changing procedure that your consultant will only suggest if the benefits outweigh the long-term impact.
Most people with pancreatic cancer are over 60. It can affect you at any age, but it’s unlikely to happen before you’re 40. It’s an age-related cancer, meaning it becomes more common with older age.
In the UK, pancreatic cancer is the 10th most common cancer. It affects around 1 in 60 women and 1 in 52 men.
How fast pancreatic cancer grows and spreads varies from person to person, and depends on the type of cancer you have. Your biopsy or surgery results may include a cancer grading or a genomic test, which are both used to predict how quickly your cancer might progress.
The best person to tell you about your pancreatic cancer prognosis is your specialist consultant, as they can consider all the individual factors that affect your outlook.
Pancreatic cancer doesn’t always cause symptoms. But some people get pain in their stomach, back, or both. It may start in the top of the stomach and spread along the sides of your abdomen or to your back.
Not everyone gets pain as a symptom of pancreatic cancer. But people who do have it describe different kinds of pain.
Pancreatic cancer pain can be:
- Mild or very severe
- Dull or gnawing
- Intermittent (coming and going)
- Worse after eating or when lying down
Always see a doctor about pain in your stomach, especially if it doesn’t go away, or gets worse.
If you have a pancreatic cancer diagnosis and you’re in pain, speak to your consultant and find out if there are other options you can try for pain management.
Useful resources
Reviewed by: Dr James Good
Clinical Oncologist
December 2024

