Everything you need to know about pancreatic health and cancer
From helping us digest our food to maintaining our blood sugar levels, the pancreas is key to making sure we feel our best. But what happens when it’s affected by cancer or other conditions? Learn more about the pancreas, pancreatic cancer and the latest treatments available at GenesisCare .
9 minute read
Introduction
According to Cancer Research UK, pancreatic cancer is the 10th most common cancer, with around 10,500 new diagnoses in the UK every year.1
One of the biggest challenges in treating pancreatic cancer is late diagnosis. Pancreatic cancer often doesn’t cause symptoms in the early stages, and, for many people, symptoms can be vague and easily attributed to less serious conditions such as indigestion. By the time symptoms are more noticeable, the cancer has grown and spread, making it harder to treat.
While early diagnosis is desirable, it may not always be possible. But, as treatment has continued to improve, there are now treatment options for all stages of pancreatic cancer.
Knowing the facts about your pancreatic health and the signs of cancer can help reduce risk and improve the chances of early diagnosis and treatment. If you’ve been diagnosed with pancreatic cancer, being equipped with knowledge about your condition and treatment options may help you feel more confident moving forward.
What is the pancreas and where is it located?
The pancreas is an organ in the digestive system that makes enzymes to break down food so the body can absorb the nutrients. It also produces hormones, including insulin, which control sugar levels in the blood. These hormones act as chemical messengers in the body and control how different organs work.
It’s about 15 cm (6 in) long and is found in your abdomen, behind the stomach and in front of the spine. A healthy pancreas is soft, smooth, and salmon pink in colour.
There are three main parts to the pancreas:
- The head – the rounded section that connects to the small intestines (duodenum)
- The body – the middle section
- The tail – the narrow section pointing towards the spleen
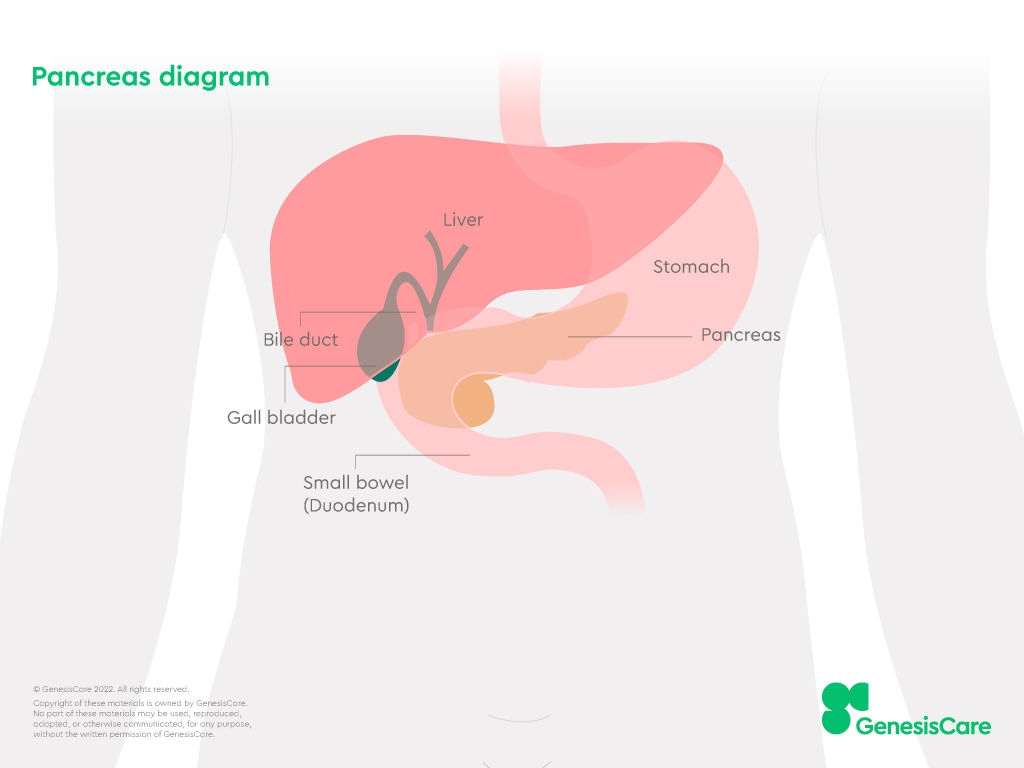
There is also a pancreatic duct, which is a tube that runs through the pancreas. This connects the pancreas to the gallbladder via the common bile duct and empties into the small intestines.
What does the pancreas do?
The pancreas plays two roles in our overall health – a digestive role and a hormonal role. Two types of cells allow it to perform these roles simultaneously. They are exocrine cells and endocrine cells.
Digestive role
When you eat a meal, your stomach sends signals to other organs in the digestive system, like your pancreas. These signals tell the exocrine cells in your pancreas to make a mixture of digestive enzymes.
The enzymes make their way through the duct to the pancreas head, where they mix with bile from the gallbladder. Together, they move into the small intestines to break down the fats, carbohydrates, and protein in your meal.
Hormonal role
Endocrine cells don’t produce enzymes. Instead, they make hormones. Hormones are chemical messengers that affect many processes in your body. The pancreas produces two hormones called insulin and glucagon, which control blood sugar levels.
Balanced sugar levels are important for the function of the body’s organs, including the brain, lungs, liver, kidneys and heart.
Improper pancreas function
If the pancreas is unable to perform as it’s supposed to, it can affect you in several ways.
These include:
- Weight loss due to a lack of nutrients
- Changes in bathroom habits (constipation, diarrhoea, greasy stools) as food isn’t digested properly
- Type 3c diabetes – a form of diabetes from pancreas damage
Conditions of the pancreas
Problems in the pancreas aren’t always caused by cancer. One condition that can cause symptoms is pancreatitis, which is an inflammation of the pancreas.
There are two types – acute pancreatitis and chronic pancreatitis.
Acute pancreatitis is sudden and short-lived. It’s a painful condition that can be serious, but most people can recover fully with hospital treatment and time.
Chronic pancreatitis involves repeated episodes of inflammation over time. This causes scar tissue to form in the pancreas, which can affect its ability to function.
Although chronic pancreatitis is rare, it’s important to diagnose as it can increase the risk of pancreatic cancer. Sometimes, pancreatitis may be mistaken for other conditions like irritable bowel syndrome.
What is pancreatic cancer?
Pancreatic cancer develops when cells in the pancreas multiply uncontrollably, forming a lump (a tumour, lesion, or mass).
There are two main groups of pancreatic cancer, depending on which cells are affected. These are exocrine tumours and neuroendocrine tumours.
Exocrine tumours start in exocrine cells and affect digestion. They’re the most common type, with 95 in 100 pancreatic cancers being exocrine, according to Pancreatic Cancer UK.2 Most cases of exocrine tumours are pancreatic ductal adenocarcinomas (PDACs).
On the other hand, endocrine tumours start in endocrine cells and affect hormone production. They are grouped into functioning or non-functioning.
- Functioning tumours produce extra hormones and cause hormonal symptoms[AO1] , which are often vague but can include high or low blood sugars, muscle weakness and skin rashes
- Non-functioning tumours do not produce extra hormones (some produce no hormones at all), so they do not cause hormonal symptoms
Most endocrine tumours of the pancreas are non-functioning. They tend to be much rarer and require a different treatment process compared to exocrine tumours.
Risk factors
Unfortunately, there are no known causes of pancreatic cancer. But there are things that may increase your risk of getting it.
Some risk factors for pancreatic cancer include:
- Older age – most people are diagnosed at 65 or older
- Regular tobacco and alcohol use
- A diet high in red or processed meats, fat, and sugar and low in fresh fruits and vegetables
- A family history
Having any of these risk factors does not mean you will develop pancreatic cancer. But avoiding some of them may reduce your chances and improve your overall wellbeing.
Symptoms
Some people with pancreatic cancer may have symptoms like:
- Pain in the abdomen and back
- Yellowing of the skin or eyes (jaundice)
- Unexplained weight and appetite loss
- Changes in bathroom habits (diarrhoea, constipation, colour, texture and odour)
- Fatigue
Other symptoms include itchy skin, fever, indigestion, and feeling and being sick.
In the early stages, many people do not have symptoms. Symptoms can come and go, not show at the same time, or be mistaken for something else. Always speak to your doctor if you have any symptoms that could be associated with pancreatic cancer.
Why is pancreatic cancer often diagnosed late?
The earlier pancreatic cancer is diagnosed, the more treatment options there are available. But, as we saw earlier, symptoms are often vague, and there may not be any until the cancer has grown and spread. This means that 8 in 10 people are diagnosed when the cancer has spread to other organs (stage four or advanced cancer), according to Pancreatic Cancer UK.
The stage describes the size and spread of the cancer.
- Stage three means it’s growing in and around the pancreas, which can sometimes lead to blockages of major blood vessels around it
- Stage four means the cancer has spread to other parts of the body, such as the liver, lungs, or bones
Compared to some cancers, pancreatic cancer can be difficult to treat. It’s often diagnosed late and is close to many delicate organs and blood vessels. However, treatments have evolved greatly within recent years, meaning late diagnosis no longer means untreatable.
What are the treatment options for pancreatic cancer?
Treatment often involves a combination of different therapy options. In addition to conventional therapies including surgery, chemotherapy, and radiotherapy, GenesisCare goes further, delivering innovative and proven radiotherapy techniques not readily available elsewhere.
Treatment plans are decided by a team of healthcare professionals which may include:
- a specialist surgeon
- oncologists (cancer specialists)
- a gastroenterologist (an expert in conditions affecting digestion)
They’ll consider your cancer stage and overall health to ensure the most suitable course of action is taken.
Surgery
Generally, surgery is only suitable in stages one or two. This is because there’s a higher chance of taking out most or all of the cancer in one operation.
Surgery may involve taking out all of the pancreas (full) or part of the pancreas (partial). The main techniques are open surgery or keyhole surgery.
The treatment your surgeon recommends often depends on the location of the cancer. For example, Whipple’s procedure involves removing the pancreas head and is usually an open surgery.
At GenesisCare, expert surgeons work collaboratively with other cancer specialists in locally and nationally renowned hospitals to decide your treatment course. If they suggest surgery, it can be conveniently arranged at one of our partner hospitals.
Chemotherapy
Chemotherapy uses cytotoxic (anti-cancer) drugs to slow the growth of cancer cells.
It can be a single drug or a combination of multiple drugs and may be offered alongside radiotherapy (chemoradiation). Your consultation team will assess your cancer and overall condition to recommend which would offer the best outcomes for you.
If you’re having surgery, you may receive chemotherapy or chemoradiation before and after your surgery. This can help shrink the cancer before the operation and reduce the chances of it returning.
Chemotherapy can also be personalised to individuals through specialist testing like genomic testing or used as palliative treatment to ease symptoms.
Radiotherapy
Radiotherapy uses targeted, high-energy radiation beams to destroy cancer cells while minimising damage to healthy tissue. As it’s highly precise, it’s often used to treat inoperable pancreatic cancer.
Some examples of radiotherapy techniques are:
- Stereotactic ablative radiotherapy (SABR) – large-dose radiation delivered to specific targets with high precision and accuracy
- Chemoradiation – a longer course of combination treatment that is sometimes used before surgery to reduce the chance of the cancer coming back afterwards
Here at GenesisCare, we offer all three options.
Advanced radiotherapy at GenesisCare
GenesisCare is a national centre-of-excellence in stereotactic ablative radiotherapy (SABR) for both inoperable and secondary (metastatic) pancreatic cancer, having treated more patients than any other centre in the UK with this technique. In addition to offering SABR across our 14 treatment centres, patients can access MRI-guided SABR– the latest technology in precision radiotherapy using the UK’s first MRIdian MR linac machines, exclusively available in the UK at our centres in Oxford and Cromwell Hospital London.
The MRIdian combines magnetic resonance imaging (MRI) with live images to accurately pinpoint the tumour location during treatment. If the cancer moves even slightly out of the target area, the treatment beam automatically shuts off to avoid damage to surrounding healthy organs, leading to fewer side effects. The MRIdian is mostly used to treat inoperable tumours, which is common in patients with pancreatic cancer. It also allows the treatment team to account for any changes in internal anatomy between treatment sessions, which maximises the chance of tumour control and minimises the risk of side effects.
MRI-guided SABR is delivered in an outpatient setting, with treatment completed in just five sessions. With this approach, patients receive effective treatment without overnight hospital stays or prolonged recovery. There is evidence that this world-class innovation in radiotherapy may be more effective than chemoradiation in prolonging survival for pancreatic cancer.
We’re the UK’s leading independent provider of cancer care, specialising in the treatment of complex cancers such as pancreatic cancer. We’re committed to offering the latest treatment innovations and techniques in cancer care to every patient – without delay.
Our teams of cancer experts are dedicated to ensuring you receive a personalised treatment plan that delivers the best outcomes possible for you and your condition.







