- Healthcare Professionals
- Resources
- Case studies
- Gastric MALT Lymphoma
Gastric MALT Lymphoma
A case study of MR-guided adaptive radiotherapy for gastric MALT lymphoma.

Case study
MR-guided adaptive radiotherapy for gastric MALT lymphoma
Dr Veni Ezhil
Dr Veni Ezhil is a Consultant Clinical Oncologist in Guildford, Oxford, and London. She specialises in respiratory motion management and advanced technical radiotherapy. She is currently the SABR lead for the treatment of oligometastases at Royal Surrey County Hospital.

Case presentation
In January 2022, a 39-year-old male presented with a one year history of nausea, abdominal discomfort, and weight loss. The patient was referred to a gastroenterologist, who performed an endoscopy and biopsied an area of thickened stomach wall which confirmed the diagnosis of marginal zone lymphoma. Sample was negative for H. pylori.
Patient was referred to a haematologist for the treatment of gastric MALT lymphoma.
A staging PET-CT scan confirmed the stomach and a small left gastric lymph node to be the only sites involved staging him IAE. Examination of the bone marrow was negative.
The patient was otherwise fit and fully active with a PS-0.
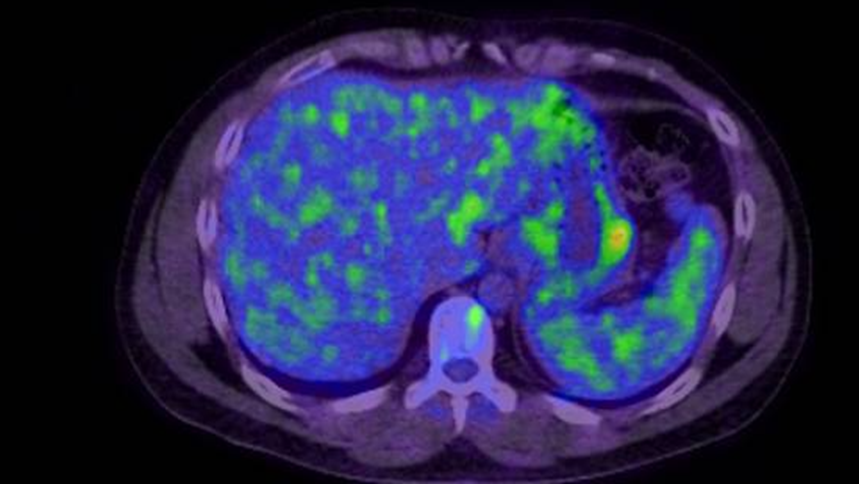
Fig 1: PET-CT showing uptake in the stomach
Patient was treated with four cycles of Rituximab to reduce the risk of distant relapse and was referred for radiotherapy to the stomach.
Challenges of presentation and choice of treatment
Radiotherapy to the stomach is challenging due to the daily changes in the shape and volume of the stomach over the course of treatment and movement of the stomach with respiration. It’s also difficult to visualise the stomach on daily non-contrast CT images on the treatment machine to guide accurate delivery of radiotherapy.
A large margin (2-3 cm) is typically applied to the stomach to overcome these challenges, resulting in a large volume of surrounding normal structures included in the radiation volume leading to increased toxicity.
MR-guided adaptive radiotherapy for gastric MALT lymphoma overcomes all the three challenges that cause concern with gastric radiotherapy, allowing for an ultra-accurate treatment delivery with reduced toxicity. The aim of this treatment method is to eradicate the disease in the stomach and achieve local control in early-stage lymphoma localised to the stomach.
Alternative treatment would have been to treat on a conventional linac using a respiratory correlated CT scan for simulation to account for motion associated with breathing and use a 2-3 cm margin to account for the daily changes in the shape and size of the stomach.
Treatment
The patient received treatment at GenesisCare, London Cromwell Hospital on the MRIdian MR linac. Treatment involved ISRT (involved site radiotherapy) to the stomach and the involved node delivering 24Gy in 12#, five days a week. An 8 mm PTV margin was given to the target to account for changes during treatment. Doses to the heart, kidneys and spleen were aimed to be kept as low as possible.
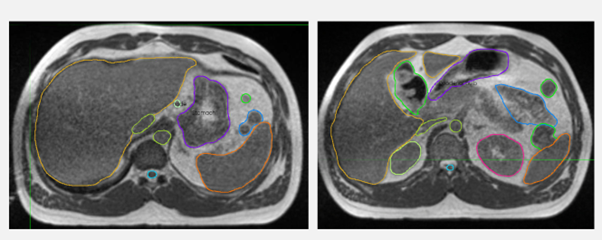
Fig 2: Planning MRI with the target and nearby organs at risk
The patient’s treatment was delivered in inspiration breath hold, tracking the stomach in real-time and delivering radiation only when the stomach was within the defined boundary. This improved the accuracy of delivery, allowing for opportunities to stop and amend where required.
On the first day of treatment, the shape and volume of the stomach was found to be very different from the planning scan. Complete recontouring was carried out to reflect the shape and volume of the stomach on the day. Surrounding organs at risk (OARs), heart, kidneys, spleen, and spinal cord, were also amended as required. The treatment plan was re-optimised to get the best dose to the target and as low dose as possible to the surrounding organs. This step overcomes the challenge of the daily change in the anatomy of the stomach.
On the second day of treatment, a gas bubble appeared during treatment which displaced the stomach out of the boundary. We were able to see this, stop treatment and recontour and plan before restarting treatment.
The target and nearby OARs were recontoured daily for all 12 fractions of treatment to accommodate the change in anatomy and the treatment plan was re-optimised to the new contours. As the size and shape of the stomach changed significantly every day, it needed complete recontouring rather than editing. The total time on bed for each session was 60 minutes.
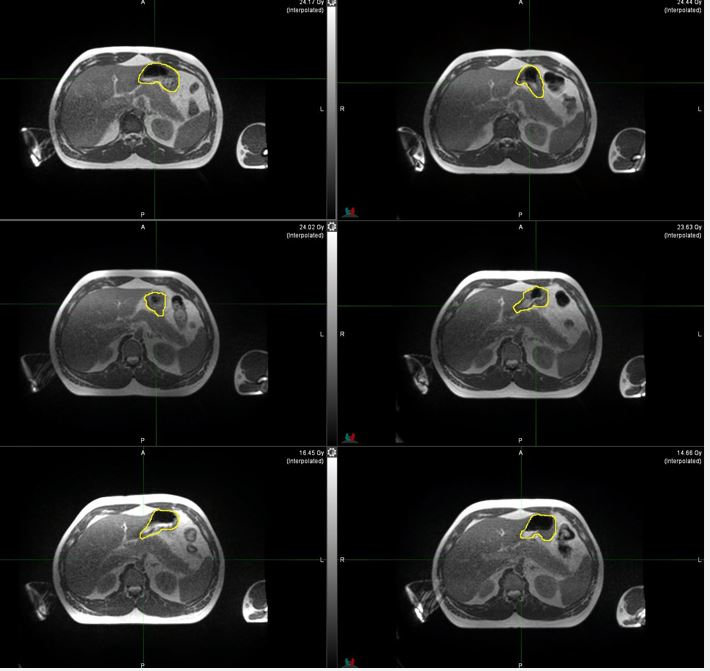
Fig 3: Change in the shape and volume of stomach at different fractions
Side effects and management
The patient experienced nausea during radiotherapy and was given prophylactic anti-sickness medications to help control this during sessions. He did report tiredness during treatment but otherwise tolerated radiotherapy well without any significant toxicity. His weight remained stable during his treatment.
Results and follow-up
The patient was reviewed at four weeks to rule out any toxicity from radiotherapy and was discharged for follow up with the haematologist.
The patient had an endoscopy three months after completion of radiotherapy to assess response which showed no evidence of lymphoma.
Discussion
This was the first case of gastric MALT lymphoma treated at GenesisCare using MR-Guided adaptive radiotherapy. We were able to accommodate the daily changes in anatomy and maximise local control and minimise toxicity.
The time on table was longer than conventional radiotherapy due to the time taken for adapting the contours and plan. With upcoming developments on MRIdian and further clinical experience we believe the time on bed can be reduced to make it easier for the patients.